What is the Highest Evidence-Based Study?
When it comes to healthcare and medical research, the quest for the highest evidence-based study often leads us to systematic reviews and meta-analyses. They stand at the pinnacle of the evidence hierarchy, providing insights and conclusions drawn from extensive research. But what exactly makes these studies the gold standard? Let’s delve into the workings of systematic reviews, understand the hierarchy of evidence, and explore how they shape clinical practice.
The Essence of Evidence-Based Medicine
Evidence-based medicine (EBM) is an integrative approach combining individual clinical expertise with the best available research evidence to improve patient outcomes. At its core, EBM seeks to provide healthcare professionals with a framework to make informed clinical decisions. Central to this framework is the hierarchy of evidence, which classifies various types of research studies according to their methodological rigor and reliability.
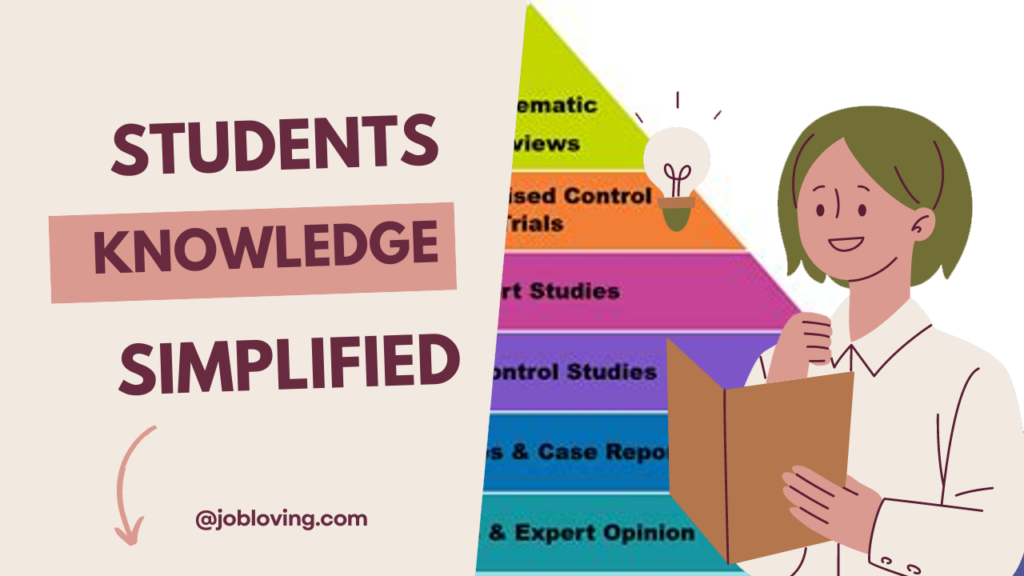
The Evidence Pyramid: Ranking of Study Types
The levels of evidence pyramid is a visual representation that illustrates the hierarchy of different types of studies. At the pinnacle, we find systematic reviews and meta-analyses. Below them are randomized controlled trials (RCTs), cohort studies, case-control studies, and finally, expert opinions and anecdotal evidence. Each layer signifies a different level of evidence quality, with systematic reviews standing out for their comprehensive evaluation of clinical questions derived from multiple studies.
| Level of Evidence | Type of Study | Description |
|---|---|---|
| 1 | Systematic Reviews/Meta-analyses | Summaries of research derived from multiple studies, providing a comprehensive evaluation. |
| 2 | Randomized Controlled Trials (RCTs) | Studies that minimize bias by randomly assigning participants to treatment or control groups. |
| 3 | Cohort Studies | Observational studies following a group over time, evaluating outcomes in relation to exposures. |
| 4 | Case-Control Studies | Studies comparing groups with and without a specific outcome to identify risk factors. |
| 5 | Expert Opinions | Insights from leaders in the field; less rigorous than systematic reviews or trials. |
The Power of Systematic Reviews and Meta-Analyses
Among various types of evidence-based research, systematic reviews are considered one of the highest forms of evidence. These reviews carefully collect, appraise, and synthesize research studies relevant to specific healthcare questions. What sets them apart? It’s their rigorous methodology that ensures reliability and validity.
Meta-analyses, a subset of systematic reviews, take this a step further by statistically combining results from multiple studies. This aggregation of data enables researchers to identify overall trends, strengths, and weaknesses of specific interventions or treatments effectively.
Cochrane Reviews: The Gold Standard
Recognized as the gold standard for systematic reviews in healthcare research, Cochrane Reviews exemplify the best practices in evidence synthesis. They adhere to strict methodological standards to minimize bias and ensure comprehensive evaluations, making them a reliable source of evidence for healthcare decision-making.
Importance of Comprehensive Literature Searches
Well-focused systematic reviews begin with thorough literature searches to capture all relevant studies. This comprehensive approach helps minimize publication bias and ensures that all evidence is considered, leading to more reliable conclusions. During this process, it is also essential to filter resources, helping researchers hone in on high-quality studies.
Why Systematic Reviews Are Essential for Clinical Practice
Healthcare practitioners rely on evidence to make informed clinical decisions. Systematic reviews serve as crucial resources that synthesize vast amounts of research, allowing practitioners to access synthesized evidence quickly. They guide best practices, inform treatment protocols, and ultimately help improve patient outcomes.
Navigating the plethora of available research can be overwhelming. With systematic reviews, clinicians can streamline their decision-making processes by relying on condensed information derived from higher-quality studies. The emphasis on filtering literature ensures that practitioners access well-conducted studies over anecdotal evidence or lower-quality research.
Ongoing Evaluation and Adaptation of Evidence
Despite the robustness of systematic reviews, science is an ever-evolving field. New studies emerge continuously, which can render previous reviews outdated. As a result, practitioners must stay vigilant and appraise new evidence to ensure that clinical decisions reflect the most up-to-date information. The responsibility lies with healthcare professionals to critically evaluate individual studies and determine their applicability to patient care decisions.
The Role of Critical Appraisal
Critical appraisal involves evaluating the credibility and relevance of research studies to ascertain if their findings can be applied to clinical settings. Systematic reviews may synthesize multiple studies, but they still require careful consideration of their individual strengths and weaknesses. Various tools and scales, such as the Jadad scale, can assist in assessing the quality of randomized controlled trials, focusing on randomization, blinding, and dropout rates.
Finding the Right Evidence: Challenges and Resources
One challenge faced in evidence-based practice is navigating unfiltered resources. These require critical appraisal to validate findings, as they may contain bias or flawed methodology. In contrast, filtering literature offers clinicians a curated collection of high-quality research that saves time and enhances the reliability of answers in critical decision-making situations.
Several databases serve as essential resources for healthcare professionals searching for evidence-based studies:
- CINAHL: Comprehensive nursing and allied health literature database.
- MEDLINE: Extensive biomedical literature, ideal for accessing clinical studies.
- JBI EBP Database: Offers systematic reviews and evidence summaries for decision-making.
- Cochrane Library: Contains high-quality systematic reviews and clinical trials.
- TRIP Database: Connects evidence-based synopses with clinical answers for practical application.
Challenges and Limitations in Evidence-Based Research
Despite the advances in evidence-based practice, challenges persist. Many studies, particularly in fields like plastic surgery, have historically suffered from inadequate quality of randomization and blinding processes. A historical analysis of plastic surgery literature revealed that in 1983, a staggering 93% of published studies were deemed low-level evidence. By 2003, only 1.5% reached the level of strong evidence (level 1). This slow progression highlights the need for continuous improvement in the quality and rigor of studies conducted in this field.
Moreover, it’s essential to note that not all clinical questions can be expertly answered by RCTs or systematic reviews. Different question types — whether relating to therapy, diagnosis, prognosis — require tailored study designs to yield optimal evidence. Hence, while systematic reviews and meta-analyses provide strong evidence, the context and nature of the inquiry are pivotal in selecting the most suitable evidence types.
Flexibility and Adaptability in Evidence-Based Practice
Incorporating patient preferences and new emerging data is vital for successful evidence-based practices. Each patient’s unique situation must guide clinical decisions, making flexibility a necessity. Rigid adherence to a single piece of evidence can lead to suboptimal patient outcomes. Practitioners should remain open-minded, continually evaluating the relevance of evolving evidence and adapting practices to suit each patient’s needs.
Conclusion: Embracing the Best Evidence
In the ongoing endeavor to optimize healthcare, the recognition of systematic reviews and meta-analyses as the highest evidence-based studies is crucial. These comprehensive evaluations synthesize multiple studies, providing practitioners with the reliability they need to make informed clinical decisions. The hierarchy of evidence, with its emphasis on rigor and methodological quality, stands as a guiding framework for evidence-based practice.
As healthcare continues to evolve, practitioners must remain committed to understanding the evolution of evidence levels, navigating resources, and integrating the best available evidence with their clinical expertise. By doing so, they enhance their ability to deliver quality care tailored to individual patients, ultimately leading to improved health outcomes.
In conclusion, the highest evidence-based study — the systematic review — is not just a collection of findings. It embodies a synthesis of knowledge, a commitment to rigorous methodology, and an essential tool for progress in clinical practice.